The 5 Elements to Avoid During your Next Dental Visit
As with any medical field, the commonly accepted principles in dentistry continue to evolve with time. With perpetual innovation and greater understanding through research, dentists are provided with greater insight for how to best care for their patients. Furthermore, within the biological dental community, practitioners are routinely searching for ways to safeguard their patient’s overall well-being in addition to their dental health. In that light, it is also vital that providers stay informed about elements of care that may pose potential harm to their patients. The following list details 5 things that both patients and practitioners should be aware to avoid during holistic dental care:
- Amalgam
- What is it?
- Dental amalgam is a liquid metal alloy mixture, the largest component of which is mercury.1-3 In dentistry, it is also commonly referred to as silver filling, metal filling, or mercury filling.
- When is it used in dentistry?
- Amalgam is often utilized for dental fillings and is found underneath older crowns and bridges. It is generally detectable based on its metallic display as a filling. However, even if the exterior of a crown/bridge presents as “white”, amalgam may still be encased underneath the restoration.
- How can it negatively impact overall health?
- The potential side effects of dental amalgam have become widely researched. Many countries have phased out dental amalgam, but 45% of all dental restorations world-wide still use amalgam.4-7 It is believed that dental amalgam fillings are continually releasing mercury when chewing, drinking, grinding, and brushing.9-10 Furthermore, the human body has difficulty destroying or detoxifying mercury. In fact, mercury is often stored within the liver, kidneys, central nervous system, large intestine, thyroid, and fatty tissue for decades.8 While not all patients experience symptoms from dental amalgam, many experience localized inflammation, chronic fatigue, limb pain, headaches, lack of concentration, memory loss, insomnia, unexplained palpitations, tinnitus, and hearing loss.11-12
- Biocompatible alternatives
- For a more holistic approach, it is recommended that all dental amalgam be removed by an IAOMT certified dentist who will perform mercury-safe removal with serious precautions (SMART protocols) to minimize exposure.13 Any mercury dentistry can then be replaced with more biocompatible (non-metal) materials.
- What is it?

- Fluoride
- What is it?
- Fluoride is a naturally occurring mineral that is released from rock formations.14
- When is it used in dentistry?
- Fluoride exposure in the United States has increased drastically since the 1940s. The main sources of fluoride include community water, soil, pesticides, fertilizers, dental products, pharmaceutical drugs, and cookware.15 In dentistry, fluoride is commonly used in-office as a topical treatment with the goal of preventing decay/cavities. In some cases, dentists may prescribe oral fluoride supplements that the patients use at home.16 Often times, fluoride is used as an ingredient in other dental products as well.
- How can it negatively impact overall health?
- Research is now indicating that excessive fluoride exposure can impact every part of the human body. Many studies have demonstrated the health risks associated with fluoride exposure.17 Some of the human health risks associated with fluoride are as follows:
- Biocompatible alternatives
- To help maintain tooth mineralization and prevent carries, many biological dentists recommend calcium, xylitol, mineral creams and oral rinses, oral powders, coconut oil, and ozone therapy.19 Additionally, for at-home oral care, several companies now make fluoride-free products that can be utilized.
- What is it?
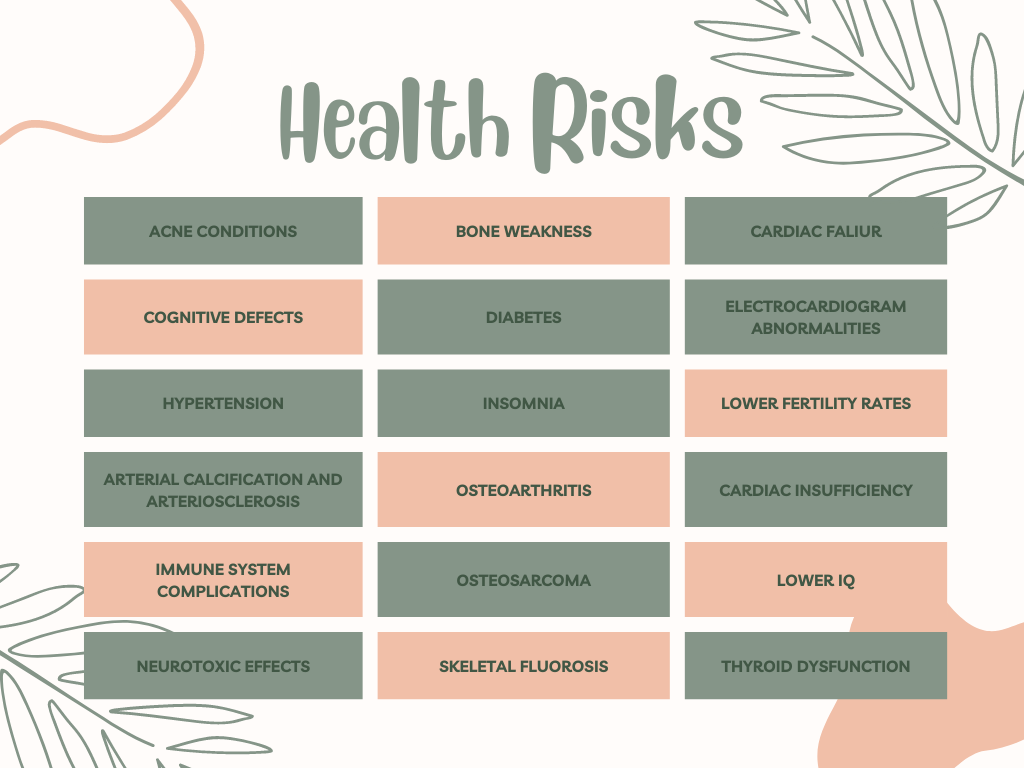
Chart derived from International Academy of Oral Medicine and Toxicology18
- Titanium Implants
- What are they?
- Titanium implants are posts created from a metal alloy that are surgically inserted into a patient’s jawbone to create an anchor for a prosthetic tooth.20
- When is it used in dentistry?
- Titanium implants are generally used to replace the absence of a natural tooth. In general, dental implants help to restore the ability to chew, assist in retaining cosmetic appearance, prevent loss of bone in the jaw, preserve the health of the surrounding gums, ensure stability of adjacent (neighboring) teeth, and often improve quality of life.21
- How can they negatively impact overall health?
- While there are certainly advantages to placing dental implants when pertinent, research is beginning to indicate that the use of titanium implants may have potentially harmful implications to whole-body health. Most individuals have a relatively low tolerance to titanium, making it largely bio-incompatible.22 Titanium implants can pose a greater risk of causing peri-implantitis due to “rusting” or corrosion.23-27 They may also cause an autoimmune reaction if they trigger the release of cytokines and instigate oxidative stress.28, 29 Based on the metallic composition, titanium can amplify magnetic waves, leading to balance distortion and systemic inflammation.30
- Biocompatible alternatives
- Many biological dentists now prefer ceramic implants to titanium implants. Ceramic implants often mimic the white, natural tooth more exactly, providing a cosmetic advantage. They are metal-free, which avoids the potential negative ramifications of titanium implants.8 They are generally made of zirconia dioxide and thus do not interfere with the energetic meridians of the body.31, 32 Research also shows that ceramic implants pose low risk of peri-implantitis resulting in healthy bone regrowth and higher long-term success rate when compared to titanium implants.33, 34
- What are they?

- High-Radiation X-Rays
- What are they?
- Dental x-rays are internal images of the mouth that are captured using electromagnetic radiation. The radiation beams pass through the soft tissues and creates an image of the teeth and bones.35 High-radiation x-rays are those that produce large amounts of carcinogens when utilized.36
- When is it used in dentistry?
- X-rays are used in dentistry to help diagnose the current status of an individual’s oral health. In the field of modern dentistry, x-rays are considered an essential diagnostic tool.35
- How can it negatively impact overall health?
- All x-rays have some level of impact on the human body. However, high-radiation x-rays are known to emit higher levels of carcinogens (cancer-causing agents). The level of radiation exposure is dependent upon the type of image being captured and the technology/equipment used to take the image. Traditional x-rays that use film to capture images are known to produce high levels of radiation, often times 80% higher than the more modern digital x-rays.37
- Biocompatible alternatives
- In order to safe-guard health, many biological dentists have begun to incorporate digital x-rays as a safer means of collecting diagnostic information. Furthermore, when capturing 3D images (which have notoriously higher levels of radiation exposure), dental patients can now benefit from low-dose radiography from x-ray machines like Green CT – Vatech.38
- What are they?

- Dental Contouring/Teeth Filing
- What is it?
- Dental contouring or teeth filing is when a dentist removes enamel from the tooth using a drill and/or laser.39
- When is it used in dentistry?
- Oftentimes, this is done in order to achieve a cosmetic goal (desired size, shape, or length).39 It is sometimes recommended as a cost effective, fast-results option for achieving aesthetic desires.40
- How can it negatively impact overall health?
- One of the main risks associated with dental contouring is the increase of tooth sensitivity (especially to hot and cold substances) which can negatively impact quality of life.41 When smoothing the contours of the natural teeth, chewing efficacy is also inhibited. This can then lead to issues with digestion and overall health. Lastly, if the tooth is filed without regard for the bite, this can lead to disruption of bite harmony and possibly to TMD (temporomandibular disorders).
- Biocompatible alternatives
- Many of the standard alternatives to dental contouring are dental bonding, veneers, and crowns.42 While these can be helpful at times, a more holistic solution (when applicable) is to utilize Bioclear. This is an innovative technique that achieves long-lasting aesthetic results, while also preserving the natural structure of the tooth.43
- What is it?
As individuals explore options for their dental vitality, we encourage everyone to consider modalities that improve their oral wellness without negatively impacting their systemic health. If you’d like to learn more about the ways in which Dr. Sharon Dickerson approaches holistic dental care, please feel welcome to contact our office at 720.842.7002.
Citations
- Ferracane, Jack L. (2001). Materials in Dentistry: Principles and Applications – Jack L. Ferracane – Google Boeken. ISBN9780781727334. Retrieved 19 September 2012.
- Mutter J. Gesund statt chronisch krank!: Der ganzheitli- che Weg: Vorbeugung und Heilung sind möglich. 3rd ed. Weil der Stadt: Fit fürs Leben Verlag; 2014. 456 Seiten. (Gesundheit).
- Mutter J, Klinghardt D. Amalgam: Risiko für die Mensch- heit; Quecksilbervergiftungen richtig ausleiten, neue Fak- ten und Hilfe, auch nach der Amalgamentfernung! 3rd ed. Weil der Stadt: Fit-fürs-Leben-Verl. in der NaturaViva-Verl.- GmbH; 2013. 169 Seiten. (Gesundheit)
- UN Environment. Global Mercury Supply, Trade and Demand. Geneva, Switzerland: United Nations Environment Pro-gramme, Chemicals and Health Branch. 2017. Available from: http://wedocs.unep.org/bitstream/handle/20.500.11822/21725/global_mercury.pdf?sequence=1&isAllowed=y. Accessed April 2020.
- UN Environment. Global Mercury Supply, Trade and Demand. Geneva, Switzerland: United Nations Environment Pro-gramme, Chemicals and Health Branch. 2017. Available from: http://wedocs.unep.org/bitstream/handle/20.500.11822/21725/global_mercury.pdf?sequence=1&isAllowed=y. Accessed April 2020.
- Health Care without Harm. Four EU countries announce plans to phase out mercury fillings [press release]. August 28, 2019. Available from: https://noharm-europe.org/articles/news/europe/four-eu-countries-announce-plans-phase-out-mercury-fillings. Accessed October 2019. Comprehensive Review of Mercury in Dental Amalgam Fillings; www.iaomt.org; Page 14
- Government of Nepal Bans Use of Mercury Dental Amalgam and Mercury-Based Equipment. September 20, 2019. Available from: https://ipen.org/news/government-nepal-bans-use-mercury-dental-amalgam-and-mercury-based-equipment. Accessed April 2020..
- Swiss BioHealth, 2020. [online] Swiss-biohealth.com. Available at: <https://www.swiss-biohealth.com/wp-content/uploads/swiss-biohealth-concept-2019-en.pdf> [Accessed 5 May 2020].
- Taskinen H, Kinnunen E, Riihimäki V. A possible case of mercury-related toxicity resulting from the grinding of old amalgam restorations. Scandinavian Journal of Work, Envi- ronment & Health [Internet]. 1989;15(4):302–4. Available from: http://www.jstor.org/stable/40965672
- Eggleston DW, Nylander M. Correlation of dental amalgam with mercury in brain tissue. The Journal of Prosthetic Dentistry. 1987;58(6):704–7. doi:10.1016/0022- 3913(87)90424-0
- Lehmann I, Sack U, Lehmann J. Metal ions affecting the immune system. Met Ions Life Sci. 2011;8157–85.
- Klinghardt D. Neural Therapy & Mesotherapy Course A: The Intensive Klinghardt Academy;201180–2.
- IAOMT, 2020. The Safe Mercury Amalgam Removal Technique (SMART). [online] IAOMT. Available at: <https://iaomt.org/resources/safe-removal-amalgam-fillings/> [Accessed 5 May 2020].
- About fluoride (2019) Centers for Disease Control and Prevention. Centers for Disease Control and Prevention. Available at: https://www.cdc.gov/fluoridation/faqs/about-fluoride.html (Accessed: February 13, 2023).
- Fluoride facts: Sources, exposure and health effects (2023) IAOMT. Available at: https://iaomt.org/resources/fluoride-facts/ (Accessed: February 13, 2023).
- Fluoride (no date) MouthHealthy. Available at: https://www.mouthhealthy.org/all-topics-a-z/fluoride/#:~:text=Your%20dentist%20may%20apply%20fluoride,a%20gel%2C%20foam%20or%20liquid. (Accessed: February 13, 2023).
- Read “fluoride in drinking water: A scientific review of EPA’s standards” at nap.edu (no date) Front matter | Fluoride in Drinking Water: A Scientific Review of EPA’s Standards |The National Academies Press. Available at: https://nap.nationalacademies.org/read/11571/chapter/1 (Accessed: February 13, 2023).
- Fluoride exposure and human health risks (2022) IAOMT. Available at: https://iaomt.org/resources/fluoride-facts/fluoride-exposure-human-health-risks/ (Accessed: February 13, 2023).
- Prescott Dentistry (2022) What are the best natural fluoride alternatives?, Prescott Dentistry. Prescott Dentistry. Available at: https://prescottdentistry.com/6-natural-fluoride-alternatives/ (Accessed: February 13, 2023).
- Center for Oral & Facial Surgery (2022) A closer look at titanium implants in San Diego, Oral Surgeons of San Diego. Center for Oral & Facial Surgery. Available at: https://www.oralsurgeonsofsandiego.com/blog/2017/06/a-closer-look-at-titanium-implants/ (Accessed: February 14, 2023).
- Center for Devices and Radiological Health (no date) Dental implants: What you should know, U.S. Food and Drug Administration. FDA. Available at: https://www.fda.gov/medical-devices/dental-devices/dental-implants-what-you-should-know#:~:text=Benefits%20of%20Dental%20Implant%20Systems,the%20surrounding%20bone%20and%20gums (Accessed: February 14, 2023).
- Schutt S, Von Baehr V. Hyperreaktivitat von Gewebemakrophagen nach Kontakt mit Titanoxidpartikeln als Ursache einer verstarkten lokalen Entzundungsreaktion bei Patienten mit Periimplantitis. ZWR – Das Deutsche Zahnarzteblatt; 2010(119):222–32.
- Barao VAR, Yoon CJ, Mathew MT, Yuan JC-C, Wu CD, Sukotjo C. Attachment of Porphyromonas gingivalis to corroded commercially pure titanium and titanium-aluminumvanadium alloy. J Periodontol. 2014;85(9):1275–82. doi:10.1902/jop.2014.130595
- Delgado-Ruiz R, Romanos G. Potential Causes of Titanium Particle and Ion Release in Implant Dentistry: A Systematic Review. Int J Mol Sci. 2018;19(11). doi:10.3390/ ijms19113585
- Safioti LM, Kotsakis GA, Pozhitkov AE, Chung WO, Daubert DM. Increased Levels of Dissolved Titanium Are Associated With Peri-Implantitis – A Cross-Sectional Study. J Periodontol. 2017;88(5):436–42. doi:10.1902/jop.2016.160524
- Fretwurst T, Nelson K, Tarnow DP, Wang H-L, Giannobile WV. Is Metal Particle Release Associated with Periimplant Bone Destruction? An Emerging Concept. J Dent Res. 2018;97(3):259–65. doi:10.1177/0022034517740560
- Apaza-Bedoya K, Tarce M, Benfatti CAM, Henriques B, Mathew MT, Teughels W, Souza JCM. Synergistic interactions between corrosion and wear at titanium-based dental implant connections: A scoping review. J Periodont Res. 2017;52(6):946–54. doi:10.1111/jre.12469
- Jacobi-Gresser E. Pathogenese der Periimplantitis. Dentale Implantologie & Parodontologie [Internet];08.2019. Available from: https://www.dimagazin-aktuell.de/implantologie/ periimplantitis/story/pathogenese-der-periimplantitis__6705.html
- Swiss BioHealth, 2020. [online] Swiss-biohealth.com. Available at: <https://www.swiss-biohealth.com/wp-content/uploads/swiss-biohealth-concept-2019-en.pdf> [Accessed 5 May 2020].
- Fujii Y. Sensation of Balance Dysregulation Caused/ Aggravated by a Collection of Electromagnetic Waves in a Dental Implant. OJAPr. 2014;02(03):29–35. doi:10.4236/ojapr.2014.23004
- Sivaraman K, Chopra A, Narayan AI, Balakrishnan D. Is zirconia a viable alternative to titanium for oral implant? A critical review. J Prosthodont Res. 2018;62(2):121–33. doi:10.1016/j.jpor.2017.07.003
- Apratim A, Eachempati P, Krishnappa Salian KK, Singh V, Chhabra S, Shah S. Zirconia in dental implantology: A review. J Int Soc Prev Community Dent. 2015;5(3):147–56. doi:10.4103/2231-0762.158014
- Cionca N, Hashim D, Mombelli A. Zirconia dental implants: where are we now, and where are we heading? Periodontol 2000. 2017;73(1):241–58. doi:10.1111/prd.12180
- Volz U, Schlomer G, Sidharta J, Haase St. Klinische Nachuntersuchung von Zirkondioxidkeramik-Implantaten -Funktion als Kalzium-Kathode. Dissertation Universitat Ulm;2006.
- Dental X-rays: Types, uses and safety (no date) Cleveland Clinic. Available at: https://my.clevelandclinic.org/health/articles/11199-dental-x-rays (Accessed: February 14, 2023).
- Do X-rays and Gamma Rays cause cancer? (no date) American Cancer Society. Available at: https://www.cancer.org/healthy/cancer-causes/radiation-exposure/x-rays-gamma-rays/do-xrays-and-gamma-rays-cause-cancer.html (Accessed: February 14, 2023).
- Digital X-rays vs. traditional X-rays (2018) Independent Imaging. Available at: https://www.independentimaging.com/digital-x-rays-vs-traditional-x-rays/#:~:text=If%20you%20have%20ever%20had,80%25%20less%20radiation%20than%20traditional. (Accessed: February 14, 2023).
- Features (no date) Vatech America. Available at: https://vatechamerica.com/products/green-ct-2#!description (Accessed: February 14, 2023).
- 5 things to know about tooth contouring (2019) Celebrity Dental. Available at: https://www.celebritydental.com/blog/5-things-to-know-about-tooth-contouring/#:~:text=During%20tooth%20contouring%2C%20the%20dentist,for%20a%20natural%2Dlooking%20shine. (Accessed: February 14, 2023).
- What is dental contouring? (no date) My Affordable Dentists @Mandurah. Available at: https://www.myaffordabledentists.com.au/mandurah-news/dental-contouring-teeth-filing (Accessed: February 14, 2023).
- Higuera, V. (2020) Teeth reshaping: Pros, cons, and more, Healthline. Healthline Media. Available at: https://www.healthline.com/health/dental-and-oral-health/teeth-reshaping#disadvantages (Accessed: February 14, 2023).
- Cosmetic dentistry options for Tooth Reshaping (2021) Dazzling Smile Dental Group Bayside New York. Available at: https://www.dazzlemysmile.com/blog/cosmetic-dentistry-options-for-tooth-reshaping/ (Accessed: February 14, 2023).
- Why bioclear (2022) Bioclear. Available at: https://www.bioclearmatrix.com/why-bioclear/ (Accessed: February 14, 2023).